
NERVE PAIN
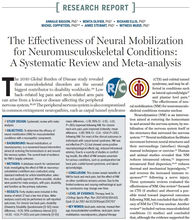
Our nerves in our body are designed to be very robust, being able to handle stretching and pressure forces on it. But once they are irritated, they can be very painful, affecting activities of daily living and cause distress. Depending on the severity, Nerve pain can often cause movement restrictions and discomfort to the neck, back, upper and lower limbs. It can also disrupt sleep and make it difficult to find positions of comfort.
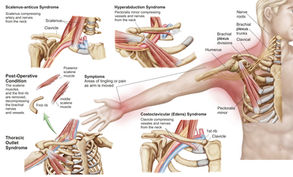
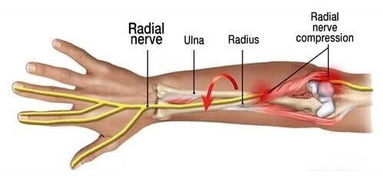
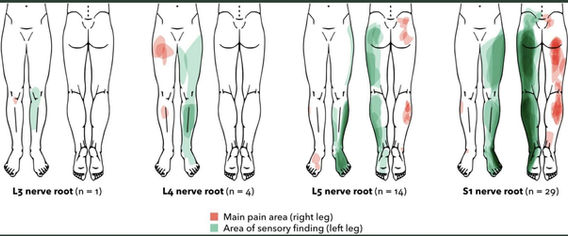
Nerve pain can often be a sharp shooting lancinating pain. Nerve pain can be classified as spinal or peripheral mediated. For instance, Sciatica / radicular pain or paresthesia (feelings of tingling, burning, numbness, altered sensation) are common terms used to describe buttock, leg or arm pain from nerve inflammation/compression originating from the lower back or neck (spinal mediated). For peripheral mediated, typically nerve pain arises from pain sensitivity in the nerves themselves e.g carpal tunnel syndrome.
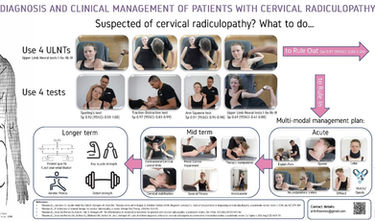
Common medical diagnostic labels for nerve pain include: radicular pain, radiculopathy that maybe caused by protrusion or prolapse of disc or spinal canal or transforaminal narrowing (i.e. stenosis) from which the nerve exits in the low back or neck; Carpal, cubital & ulnar tunnel syndrome, thoracic outlet syndrome.







Most nerve pain cases are linked to nerve inflammation. This is where painful nerves / nerve roots are inflamed but there is no compression stress. In this case, radicular pain will be present (i.e neck arm pain & between shoulders ), but no neural tissue conduction loss (i.e. muscle power, sensation and reflexes are normal). This indicates neural tissue functioning well and condition is not serious.
In situations where neural tissue is compressed, there will be neural deficits (i.e. numbness, muscle power and/ or reflex loss). This is more serious and requires urgent appropriate care. Urgent medical attention is needed for progressive loss of muscle power affecting walking and balance, genital area numbness with inability to pass urine.
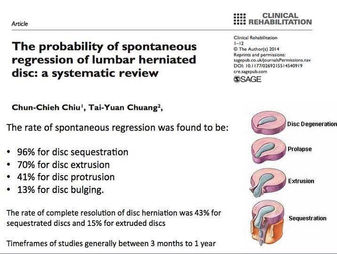
Generally, the natural healing of nerve pain conditions are good, with substantial improvements at 4-6 months +/- residual pain & minimal disability. For persistent pain cases not responding to conservative care, medical intervention is required.
Note: Neuropathic pain disorders affecting spinal cord and brain is not discussed in this section.
NERVE PAIN GALLERY







FREQUENTLY ASKED QUESTIONS

Available Soon
Additional resource will be available soon

Available Soon
Additional resource will be available soon

Available Soon
Additional resource will be available soon